Warning
This document is current with effect from the date shown on the cover page. As the International Mine Action Standards (IMAS) are subject to regular review and revision, users should consult the IMAS project website in order to verify its status at (http://www.mineactionstandards.org/, or through the UNMAS website at http://www.mineaction.org)
Copyright notice
This UN document is an International Mine Action Standard (IMAS) and is copyright protected by the UN. Neither this document, nor any extract from it, may be reproduced, stored or transmitted in any form, or by any means, for any other purpose without prior written permission from UNMAS, acting on behalf of the UN.
This document is not to be sold.
Director
United Nations Mine Action Service (UNMAS)
UNHQ
DC-2, 14th Floor, Two UN Plaza
New York
United States
Telephone: +1 (212) 963 0691
Foreword
International standards for humanitarian demining programmes were first proposed by working groups at an international technical conference in Denmark, in July 1996. Criteria were prescribed for all aspects of demining, standards were recommended and a new universal definition of ‘clearance’ was agreed. In late 1996, the principles proposed in Denmark were developed by a UN-led working group and the International Standards for Humanitarian Mine Clearance Operations were developed. A first edition was issued by the UN Mine Action Service (UNMAS) in March 1997.
The scope of these original standards has since been expanded to include the other components of mine action and to reflect changes to operational procedures, practices and norms. The standards were re-developed and renamed as International Mine Action Standards (IMAS) with the first edition produced in October 2001.
The United Nations has a general responsibility for enabling and encouraging the effective management of mine action programmes, including the development and maintenance of standards. UNMAS, therefore, is the office within the United Nations responsible for the development and maintenance of IMAS. IMAS are produced with the assistance of the Geneva International Centre for Humanitarian Demining.
At the time of writing, the World Health Organisation is finalising its "Standards for Pre-Hospital Care". These standards are expected to become a normative reference for this IMAS as they are particularly relevant to the definition of the Intermediate Care Provider. In the interim, the Technical Working Group has published TNMA 10.40 which contains a competence framework outlining basic standards that are understood and accepted across the mine action sector today.
The work of preparing, reviewing and revising IMAS is conducted by technical committees, with the support of international, governmental and non-governmental organisations. The latest version of each standard, together with information on the work of the technical committees, can be found at www.mineactionstandards.org. Individual IMAS are reviewed at least every three years to reflect developing mine action norms and practices and to incorporate changes to international regulations and requirements.
Introduction
IMAS 10.10 outlines the responsibilities of the National Mine Action Authority (NMAA), employers and employees for providing and maintaining a safe work environment. This goal is achieved through the development of safe work practices and operating procedures, effective supervision and control, appropriate education and training for both men and women, safe equipment and the provision of effective and suitable Personal Protective Equipment (PPE).
These measures will reduce the likelihood of harm, but there will always be the potential for accidents to occur in environments contaminated with explosive hazards. Demining organisations and employees must therefore be properly trained and equipped to respond. Demining is often conducted in an environment degraded by conflict and other humanitarian challenges, perhaps made worse through natural disasters. Under these circumstances diseases such as malaria, tuberculosis, trypanosmiasis and cholera, previously kept in check by national medical control measures, can again become widespread.
Developing a capacity to provide an appropriate response to a demining accident requires good planning, well trained staff and the availability of medical services able to provide effective emergency treatment. Notwithstanding the legal and moral obligations placed on managers to provide the best medical support possible, especially at the demining worksite, planning must acknowledge the reality of field operations. In explosive ordnance-affected countries suffering from post-conflict trauma, the medical facilities will often be limited, and overstretched. In these circumstances, mine action authorities and demining organisations should be as medically self-sufficient as possible in providing on-site medical support and training staff to meet the necessary competences.
New trauma treatment methodologies have been developed, and are now widely accepted, since this document was last issued. These have been discussed by a technical working group considering clinical competences under the umbrella of this document. More detailed sections on assessing a host nation’s medical facilities and occupational health have been added to acknowledge the gradual increase in best practices across the sector.
The World Health Organisation (WHO) is compiling a set of minimum standards for pre-hospital care worldwide. It is anticipated that these will become the key normative reference for this document. The standards were work in progress at the time this document went to print, but associated teaching materials have been produced by WHO and these are referenced in Annex A.
The aim of this standard is to provide greater specification and guidance for the provision of appropriate medical support to demining operations in the field. The document is in three parts: Sections 1 to 3 define the scope, references and terms used in the standard; Sections 4 and 5 define the requirements, specifications and responsibilities; and the Annexes provide references and additional detailed information and guidance on how to apply the standard.
1. Scope
Within humanitarian mine action, no worksite, setting or security situation is identical, precluding the blanket use of set procedures and timelines. That said, humanitarian mine action organizations have a responsibility to provide, or ensure access to, appropriate medical support for their staff.
This standard provides specifications and guidelines for the development of medical support to demining operations. It identifies the minimum requirements for medical emergency preparedness, including the planning required before staff deploy on demining operations, and the training of demining and medical support for male and female staff.
2. References
A list of normative references is given in Annex A. Normative references are important documents which are cited in this standard.
3. Terms, definitions and abbreviations
A complete glossary of all the terms, definitions and abbreviations used in the IMAS is given in IMAS 04.10. In the IMAS, the words 'shall', 'should' and 'may' are used to indicate the intended degree of compliance.
- 'shall' is used to indicate requirements, methods or specifications that are to be applied in order to conform to the standard;
- 'should' is used to indicate the preferred requirements, methods or specifications; and
- 'may' is used to indicate a possible method or course of action.
The term 'National Mine Action Authority' (NMAA) refers to the government entity, often an interministerial committee, in an EO-affected country charged with the responsibility for broad strategic, policy and regulatory decisions related to mine action.
Note: In the absence of an NMAA, it may be necessary and appropriate for the UN, or some other body, to assume some or all of the responsibilities of an NMAA.
The term 'demining organisation' refers to any organisation (government, NGO or commercial entity) responsible for implementing demining projects or tasks. The demining organisation may be a prime contractor, subcontractor, consultant or agent.
The term 'accident' refers to an undesired event, which results in harm.
The term 'incident' refers to an event that gives rise to an accident or has the potential to lead to an accident.
The term ‘demining accident’ refers to an refers to an accident at a demining workplace involving an Explosive Ordnance mine, and or ERW hazard (c.f. mine accident).
The term 'demining incident' refers to an incident at a demining workplace involving an explosive ordnance hazards (c.f. mine incident).
The term 'mine incident' refers to an incident away from the demining workplace involving a mine or explosive hazard (c.f. demining incident).
The term 'demining accident response plan' refers to a documented plan developed for each demining workplace which details the procedures to be applied to move victims from a demining accident site to an appropriate treatment or surgical care facility.
The term ‘competence’ refers to the ability of an individual to perform a task.
The term ‘currency’ refers to the familiarity that an individual has with a task and associated equipment. It can be thought of as “up-to-date-ness” or whether an individual is “in-date”.
The term ‘defined period’ refers to a set length of time, measured in minutes, enshrined within an organisation’s standard operating procedures, or in a worksite-specific demining accident response plan.
3.1 The chain of casualty care
For the purposes of this document, the definition of the chain of casualty care is set out in the following diagram. This is a generic and simplistic model which will not hold in every situation, but which contains therein the key elements considered in this document.
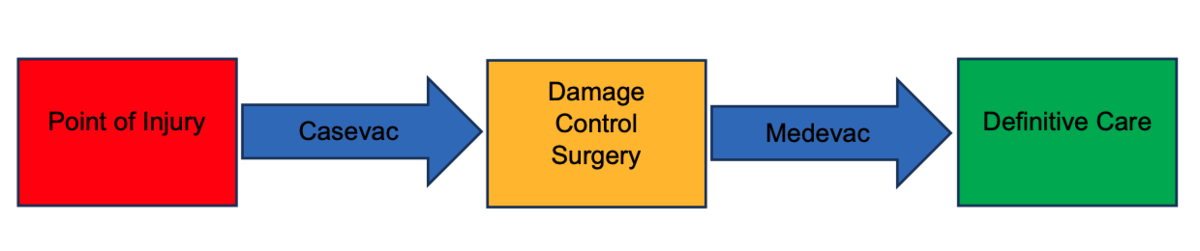
Casevac refers to the movement of the casualty and first responder colleagues out of the hazardous area and through immediate first aid and ambulance transfer to a destination at which, if basic surgery and diagnostics (including x-ray) are available, damage control surgery can be conducted. From this point, medevac refers to more deliberate operation of moving the casualty under skilled medical supervision (i.e. intubated patient under anaesthesia) to a place where ongoing care can be provided.
3.2 Medical skill levels
A framework of Basic, Intermediate and Extended Care Providers for Mine Action is provided in TNMA 10.40/01. The provision levels are a hierarchy, with an Intermediate Care Provider able to fulfil the role of a Basic Care Provider and an Extended Care Provider able to fulfil the role of an Intermediate Care Provider.
3.2.1 Basic Care
All demining and support staff working at a worksite shall be qualified and up-to-date Basic Care Providers.
3.2.2 Intermediate Care
The demining organisation shall provide someone suitably trained and qualified in the relevant competencies as an Intermediate Care Provider (ICP) within a defined period of an accident occurring.
Intermediate Care Providers are personnel meeting the minimum level of clinical competency (haemorrhage control, airway management and patient management) recommended for the provision of on-scene, immediate trauma medical care. ICPs should act as dedicated standby medical personnel or may fulfil a dual role in low-risk clerical duties outside the active worksite. If ICPs are obliged to fulfil a dual role in daily clearance, at least 1 in 4 members of clearance personnel shall be trained to the level of ICP and at least 2 ICPs shall be present on the worksite and suitably separated during periods of work.
3.2.3 Extended Care
The demining organisation shall ensure that casualties have access to an Extended Care Provider within a defined period of an accident occurring (and ideally within the “golden hour”). In many cases, Extended Care Providers will be employees of, and located in, third-party fixed medical facilities.
Extended Care Providers are experienced medical professionals that have undergone formal, and relevant, pre-hospital medical training and therefore have a much more comprehensive clinical understanding and associated scope of medical practice and response than ICPs.
3.2.4 Advanced life support
“Advanced life support” in this context is considered a methodology rather than a course and encompasses all advanced interventions after basic life support has started. The aim is to set standards of resuscitation of the trauma victim such as supporting the airway with surgical procedures (cricothyrotomy) or chest tube insertion, including the use of specific drugs. Depending on the context, these procedures may be carried out by either an ICP or ECP.
3.2.5 Damage control surgery
Damage control surgery is designed to prioritize short-term physiological recovery over anatomical reconstruction in the seriously injured and compromised patient. It allows non-surgical medical personnel (e.g. a doctor with good surgical competences) to control severe bleeding and it is part of the larger concept of Damage Control Resuscitation.
3.2.6 Definitive care system
The designated trauma care facility, either in host nation or elsewhere, identified and written in the demining accident response plan or national SOP, at which an injured staff member would be expected to receive all proper surgical interventions following a demining accident.
3.3 Defined periods: medical response timelines
Demining organisations shall have clearly stated organisation-wide goals for the provision of medical care within fixed response times, e.g. “An Intermediate Care Provider within five minutes”.
Demining organisations’ medical coordinators shall define the response times for care provision in the demining accident response plan for the worksite.
4. General Requirements
4.1 Planning and Preparation
4.1.1 Assessment
The first step in the provision of this support is a thorough assessment of existing facilities, the skills of medically trained personnel, and the availability of drugs and equipment. A demining organisation’s medical coordinator or specialist shall conduct and document a ‘baseline’ assessment of medical resources within the planned area of operation prior to the commencement of demining activity and review this at least annually. Such an assessment is the start point for adaptation of a demining organisation’s existing medical guidelines.
4.1.1.1 Medical skill levels
The assessment phase will allow demining organisations’ medical coordinators to identify skill and capability gaps within the existing medical framework and put in place mitigations where appropriate.
During programme setup, potential Intermediate and Extended Care Providers (and facilities) should be evaluated by the medical coordinator and attention should be paid to trauma or emergency room competence, rather than general health system experience.
When recruiting Intermediate Care Providers organizations should be mindful of draining potentially scarce resources from public health facilities and consider provision of ab initio training to ensure sufficient capacity to support their operations. Where organizations choose to recruit ICPs with previous medical training their trauma and emergency room competences should be assessed, and consideration given to the running of a specific trauma course.
4.1.1.2 Mapping
The medical coordinator or specialist shall map the location of all relevant medical facilities in the region in which the demining activity is planned to take place. It shall also establish the transit times between the work sites and medical facilities considering all likely traffic levels and using the appropriate medically equipped vehicle. Consideration should be given to roadblocks, hospital security access protocols and other specific issues that will affect transit time.
The mapping shall accurately establish the level of medical provision at each point and should involve a detailed professional assessment through visits to the facilities.
4.1.1.3 Casevac
Casevac shall be planned and briefed before work starts on site. Plans shall be rehearsed and re-briefed at least once a month and a clinical component should be included to ensure the maintenance of clinical skill levels.
Demining organisations shall consider the level of care to be provided to the casualty in transit during this phase, based on vehicle and terrain factors and relevant hospital / clinic operating hours.
4.1.1.4 Advanced life support
The selection of an appropriately equipped location at which to conduct advanced life support is critical to the likely survival of the casualty. Demining organisations shall balance the requirement to improve existing local facilities or provide another means of carrying out advanced life support closer to the worksite.
4.1.1.5 Medevac
The move to definitive medical care should be pre-planned but may be planned in detail during the casevac and stabilisation phases, based on medevac options established during the mapping process.
4.1.1.6 Definitive Care
The selection of a Definitive Care facility shall be carried out prior to the commencement of demining operations in a new area. In many cases the location of a suitable facility may be many hours or days transit from the worksite, and this may necessitate allocating medical resources and care providers earlier in the chain of casualty care, closer to the point of injury.
Appendix B outlines categories of definitive care facilities. Trauma care should include the following sub specialisations:
- Orthopaedics
- Neurosurgery
- Reconstructive surgery
- Anaesthesia
- Rehabilitation
It is possible that Definitive Care is available only a short distance further on from the Advanced Life Support facility. In this case, common sense may dictate that casevac should be direct to the higher-grade facility.
4.1.2 Demining accident response planning
A demining accident response plan is the detailed, tailored response of the demining organisation to the assessment phase described above. Such plans shall be developed and maintained for each demining worksite and should extend national or programme level medical SOPs, the latter being the basis for accreditation of the demining organisation by the NMAA.
The plan shall include a summary of the assessment phase as the baseline upon which care provision is detailed. Mitigations pertinent to the demining programme’s regional and local context should then be clearly explained. It is self-evident that demining organisations should establish good links with the local hospital / clinic to ensure the smoothest possible care provision in an emergency.
A combination of programme SOP and the site-specific demining accident response plan shall identify:
- the training and qualification needs of all employees at the demining worksite, i.e. workers and medical support staff with responsibilities for casualty evacuation and initial treatment;
- the equipment and materials required to implement the demining accident response plan, including: first aid and medical equipment, supplies and drugs; transportation required to move victims from the accident site to medical facilities offering treatment; and communications equipment to call forward assistance and/or to provide details of the nature and extent of injuries; and
- the location of a definitive care facility. Mine accident injuries are often severe and may require specialist surgery. The nearest suitably equipped and staffed hospital may be in the country capital, or even in a neighbouring country. If deemed appropriate, the facility should be informed of the demining activity before it commences.
4.2 Evacuation
The following section outlines a generic evacuation process and does not cover every worksite or situation. Attention should be paid to the use of “shall” and “should” in this section and the reader is encouraged to intelligently apply the best practice appropriate to their situation.
4.2.1 Extraction from hazardous area
Extraction of the casualty from the hazardous area and from further danger shall be carried out as rapidly as possible. The amount of safely accessed space around a casualty will, by necessity, determine how many staff can assist. The minimising of risk to other staff shall be a priority of the worksite manager. Care providers should not be exposed to increased risk of injury by treating a casualty in situ unless in specific, pre-determined and mitigated circumstances1. Even control of catastrophic haemorrhage may be delayed if doing so puts others at risk of injury.
The variety of techniques within demining preclude the mandating of set procedures for evacuation. An area being cleared in multiple parallel lanes will require different extraction techniques to one being worked in a single lateral (“crab”) lane. Similarly, terrain, access and vegetation on a worksite will shape the action required in the event of an accident. These factors shall be considered as part of an assessment prior to the commencement of demining activity. They shall also be outlined in the Demining Accident Response Plan and rehearsed prior to and regularly during the period of demining activity.
“Spot tasks” such as unexploded ordnance or improvised explosive device disposal tasks have hazardous areas of varying shapes around them. Marking of such areas shall be unambiguous and well-understood by all demining employees. The size and shape of the area that can be safely accessed will determine how the responding care providers access the casualty.
Where a casualty has slipped, walked, or been blown into, an uncleared area, a deliberate operation may be needed to extract them. Demining organisations shall detail the procedure to be followed when this occurs within the Demining Accident Response Plan, or in the programme level SOPs if appropriately dealt with therein.
In the event of a demining accident, a simple visual system to identify who has been involved in the accident should immediately follow. The aim of such a system is to reduce confusion and manage the complexity of the situation. On a large worksite this should be done on a team or sector basis. On a single item spot task, there may be only one person at risk.
When the casualty has been identified, the worksite manager must perform an immediate assessment of the situation and assign appropriate resources to respond.
4.2.2 Basic Care Provision
All demining and support staff working at, or nearby in support of, a worksite shall be qualified and up-to-date Basic Care Providers.
Once the casualty (or casualties) have been identified and an assessment of the safety of the scene has been made, the nearest staff member(s) should be directed to extract the casualty from the hazardous area to a safe area and apply immediate medical interventions (e.g. haemorrhage control, airway, safe-secure position and fracture stabilisation), commensurate with their training and equipment. As soon as the casualty is in a safe area, other team members can begin to assist.
The dispersed nature of a demining worksite demands that all staff shall be at an appropriate basic competence level so that immediate care can be consistent and guaranteed. Demining organisations shall be required to demonstrate evidence of up-to-date continuation training for all staff.
4.2.3 Intermediate Care Provision
All clearance teams shall have access to at least one Intermediate Care Provider within a specified response time.
The high level of competence and necessary currencies (whether they are “up-to-date”) demanded of an Intermediate Care Provider means that they will probably need to be a full-time nurse or paramedic. Demining organisations may have one Intermediate Care Provider to cover multiple worksites in the same local area provided that the communications and transport provision permits the ICP to respond within defined timescales.
Intermediate care should be capable of being provided in a fixed location or whilst mobile.
4.2.4 Extended Care Provision
The high level of competence of the Extended Care Provider demands equipment and drugs (requiring cold chain logistics) that are often found only in fixed facilities.
Extended care provision broadly aligns with advanced life support, defined in Section 3. It is unlikely that a demining organisation will directly employ an Extended Care Provider (ECP) unless they are operating in very remote areas. When operating in areas where casevac would be protracted, careful consideration must be given to the possibility of directly engaging a suitably qualified and experienced ECP, equipping the facility from which they will operate, and the associated onward medevac options.
In addition to serving the demining workforce, ECPs can facilitate medical capacity building in the community surrounding the demining workplace. In such circumstances, demining organisations should be encouraged to seek medical partner organisations so that cost can be shared, and benefit increased.
4.2.5 Damage control surgery
Whether or not a distinct damage control surgery phase takes place before a casualty is taken to an appropriate casevac destination for Definitive Care will depend on a multitude of factors. Mechanism, severity, and time of injury, local medical provision and the security situation will all require active consideration during a casevac.
4.2.6 Casevac by vehicle
After interventions to deal with the most life-threatening issues, such as haemorrhage and airway management, movement of the casualty towards a facility that can provide advanced life support shall be carried out without delay unless a care provider capable of delivering advanced life support is available on scene. In such a case, casevac may be deferred.
Movement of the casualty for anything other than a short transit shall be under the supervision of a suitable care provider who can administer appropriate medical treatment.
The nature of vehicle movement in austere environments will determine how the casualty is cared for during transit and this may demand periodic halts to allow for accurate casualty monitoring.
4.2.7 Medevac
A distinct medevac phase is clearly not required if a casualty is moved directly to an appropriate medevac destination that is able to provide Definitive Care. This is, however, not guaranteed when injuries are severe, so medical coordinators and worksite managers shall make every effort to integrate with a suitable health care provider or other agency to provide effective onward medevac. Since this may require air travel and cross-border movement, the casualty shall be appropriately equipped with the documentation to enable onward travel, prior to the conclusion of damage control surgery.
4.2.8 Definitive Care
Appropriate Definitive Care facilities may not be found within the area (or even the country) where demining activity is taking place. In this case it may be difficult for a medical coordinator to visit the appropriate facility. Selection of the Definitive Care facility should be done with due diligence on the part of the demining organisation and the relevant care standards assessed through international medical reporting.
A Definitive Care Facility shall meet the requirements detailed in the check list at Annex B.
4.3 Training
4.3.1 New Methodologies
Whilst mine action medical working groups will consider operational experience in related contexts, NMAAs and demining organisations should be encouraged to keep their procedures under regular review to reflect new findings and threats and incorporate clinical advances where appropriate.
Trends of injury type and mechanism can change over the period of a decade or less, as for example the emphasis of different operational areas moves from AP mine injuries to those caused by IEDs. The importance of generating a body of quantitative evidence to assist in evaluating the relevance of new clinical methods cannot be overstated and demining organisations shall report accidents in accordance with IMAS 10.60 even if the requirements extend those laid down by the NMAA.
4.3.2 Being up to date (currency)
Being up to date in a competence is as important as the initial training itself. On extended mine action programmes, skill fade in medical competences is a significant risk, particularly at the Intermediate Care Provider level where clinical practice hours are likely to be very low.
Demining organisations shall conduct refresher training to a pre-defined schedule. They should also conduct focused refresher training based on skill fade observed during rehearsals and casualty simulations. Demining organisations shall also conduct continuation training as required to ensure that best practice is maintained as advances in procedures and treatments are made.
All refresher and continuation training shall be recorded by the demining organisation as evidence of ongoing institutional medical competence.
Demining organisations may elect to rotate Intermediate and Extended Care Providers through posts or internships at medical facilities that experience a higher number of casualties and where clinical practice hours may be “topped up”.
4.3.3 Group currency
A well-practiced casevac is greater than the sum of its parts. The documentation of individual competences simply to achieve a declared standard of medical cover has limited value without collective rehearsal.
Suitable blood donors from the team (or victim’s family) should be identified and may travel with the casualty if such a requirement is identified in the accident response plan.
In order to ensure that the best medical response is available to an injured demining worker, regular group training shall be undertaken at least once a month.
Demining organisations shall simulate casualty evacuation and treatment, and should simulate multi-casualty evacuation, from a notional point of injury to the appropriate medical facility as part of refresher training.
4.4 Evaluation
4.4.1 Qualifications of evaluators
Deminer and paramedic quality assurance personnel should be experienced professionals who are brought in from other programmes or organisations to conduct evaluations and be able to recommend areas for improvement. Although such activity should be coordinated by the NMAA as part of the accreditation process, it should not be assumed that the NMAA will have suitable assessors available.
4.4.2 Moulage, rehearsal and casualty simulation
When creating a scenario in which to test casualty evacuation and medical care provision, it is important not to emphasise the deminer-led activity of evacuation from the hazardous area at the expense of the medical care provision. Both elements are vital to a successful accident response.
Demining organisations shall carry out regular, varied and realistic casualty evacuation rehearsals that include medical care requirements that challenge BCP and ICP levels of skill.
Rehearsals shall include the vehicle casevac phase whenever possible and should be observed by suitably qualified quality assurance personnel and by the NMAA as part of accreditation.
4.5 Occupational Health
Demining organisations can assure employee resilience, commitment and effectiveness by adopting simple preventative occupational health planning into their operational decision making. The following section builds on the general requirements laid down in IMAS 10.10.
4.5.1 Staff Medicals / Check-ups
Staff (both local and expatriate) employed by demining organisations should be assessed to determine whether they are physically and psychologically fit to conduct their designated role before deployment, and at appropriate intervals thereafter. Basic medical assessment should include blood group assessment and relevant screening for conditions that may pose a risk to others as well as a mental health baseline assessment. All staff should be subject to routine medical check-ups.
4.5.2 Heat injury
Active management of heat injury risk is required in many demining contexts. By taking a system-wide view of the problem, from working hours and rest periods to logistic supply of water, oral re-hydration salts and shelter, demining organisations shall take all reasonable measures to minimise heat injury risk.
4.5.3 Insect & animal bites
Insects and animals can be a common but serious hazard around demining operations and in workforce accommodation facilities. The preventative and responsive actions taken by the demining organisation shall be detailed in the Demining Accident Response Plan. Education of demining workers should be carried out upon induction so that frequency of incident occurrence can be minimised, prophylactics taken when appropriate, and the post-exposure procedures are widely known and understood.
4.5.4 Road Traffic Accidents
The statistical prevalence of road traffic accidents worldwide demands that demining organisations plan preventatively to minimise the hazard to staff. Safe driving techniques should be taught along with an appreciation of vehicle standards and maintenance. Where route selection can reduce risk exposure this should be considered, and, when there are safety or efficiency advantages, the demining organisation should consider improving access routes to worksites. Demining organizations should also consider including road traffic accident scenarios when providing medical training to staff.
4.5.5 Illness
Keeping track of infectious diseases, bites and other illnesses not directly related to the activity of demining or driving is important to maintain a high standard of workforce occupational health. By concentrating on mitigating the causes of such illnesses, a demining organisation can improve employee resilience, commitment and effectiveness.
Demining organisations should maintain a record of all illnesses experienced by their workforce whilst in their employ.
4.5.6 Long term illness
The duty of care of a demining organisation towards its employees should extend beyond the period of employment when an illness or impairment can be linked to the activity that was carried out during the period of employment.
Whilst the legal framework of the nation in which demining activity is taking place will drive a demining organisation’s appetite for addressing employee long-term illness, organisations shall record all details (roles, incidents, exposure etc) in an individual employment history and this should be shared with the employee at regular intervals and upon termination of the period of employment.
4.5.7 Mental Health
Mental health has often been ignored by demining organisations around the world. The long-term effects of trauma, often encountered in demining operations, can be difficult to define, especially where there is no visible physical injury to a person.
Demining organisations shall ensure that all staff required to work in hazardous areas are in good mental health. Mental health assessment should form part of the regular medical check-up.
Demining organisations should ensure that all staff involved in, or affected by, a traumatic incident are counselled and monitored in subsequent months and years.
4.6 Reporting
Reporting requirements for demining accidents and incidents are mandated in IMAS 10.60, to include the sharing of anonymized accident/incident information in-country by demining organizations and the NMAA.
Demining organisations shall decide whether to record occupational health data internally and subsequently whether to share it with other organisations. The maintenance of a detailed risk register in which identified risks are recorded along with the efforts to avoid or minimise the consequences of the risks is recommended because it is of proven benefit to risk management efforts.
5. Responsibilities
5.1 National Mine Action Authority (NMAA)
The NMAA shall:
- In conjunction with appropriate health authorities, establish and maintain documented standards and procedures for medical support to demining operations;
- monitor demining organisations’ development and maintenance of demining accident response plans;
- assist in the co-ordination of appropriate responses to demining accidents, including supporting demining organisations in overcoming security constraints in the execution of a response plan;
- assist in coordination with the health ministry, public health facilities and other relevant government agencies that may be able to provide support to accident response;
- evaluate the effectiveness of emergency response plans and assist in implementing appropriate corrective action;
- establish and maintain standards and procedures for the investigation of demining accidents; and
- establish and maintain gender-appropriate and gender-equal standards of insurance cover for medical treatment and compensation of male and female staff. This shall explicitly cover pregnancy.
5.2 Demining organisations
Demining organisations shall:
- develop and maintain Standard Operating Procedures (SOPs) which aim to reduce the risk of demining accident and incidents occurring;
- develop and maintain SOPs which aim to reduce the risk of harm resulting from demining accidents;
- develop and maintain demining accident response SOPs at programme level and demining accident response plans for each demining worksite;
- provide the training and resources needed for the implementation of the demining accident response plan; and
- ensure that demining accident response plans are practised at the minimum intervals laid down in this document.
Deming organisations should ensure that employees understand that they should:
- apply SOPs which aim to reduce the risk of a demining accident or incident;
- apply SOPs which aim to reduce the risk of harm resulting from a demining accident;
- develop and maintain skills needed to respond to demining accident emergencies;
- identify and report opportunities to improve work practices to reduce the risk of a demining accident or incident occurring and to improve the organisation's demining accident response plan; and
- carry out all the actions recommended by the medical authorities for the maintenance of occupational health.
In the absence of a NMAA, the employer shall assume additional responsibilities. These include, but are not restricted to:
- issue, maintain and update their own regulations, codes of practice, SOPs and other suitable provisions on medical support;
- cooperate with other employers or organisations in the same country to ensure consistency of standards for accident prevention, emergency procedures and occupational health; and
- assist the host nation, during the establishment of a NMAA, with assistance in framing national safety and occupational health regulations and codes of practice for all aspects of medical support.
Footnote
1 This document covers the full spectrum of humanitarian demining operations, not only minefield clearance. Spot EOD tasks, battle area clearance, IED Disposal and stockpile management operations are all addressed by this document and each one requires tailored SOPs to cover this situation.
Annex A (Normative) References
The following normative documents contain provisions, which, through reference in this text, constitute provisions of this part of the standard. For dated references, subsequent amendments to, or revisions of, any of these publications do not apply. However, parties to agreements based on this part of the standard are encouraged to investigate the possibility of applying the most recent editions of the normative documents indicated below. For undated references, the latest edition of the normative document referred to applies.
- WHO Standards for Pre-Hospital Care. These are work in progress but it is anticipated that these will become a key normative reference when published. Teaching material is available in the interim at https://www.who.int/publications-detail/basic-emergency-care-approach-to-the-acutely-ill-and-injured which is an “open-access training course for frontline healthcare providers who manage acute illness and injury with limited resources”. The slide below lists the following essential skills:

- US DoD Joint Trauma System / Ranger TCCC – data-driven approach to driving down preventable death: http://jts.amedd.army.mil/index.cfm/committees/cotccc
- The clinical competencies recommended for Basic Care Providers are informed by the Committee for Tactical Emergency Casualty Care (C-TECC 2016)
Annex B (Informative) References
Primary-level hospital: few specialties—mainly internal medicine, obstetrics and gynecology, pediatrics, and general surgery, or just general practice; limited laboratory services available for general but not specialized pathological analysis. Alternative term: District hospital-Rural hospital-Community hospital
Secondary-level hospital: highly differentiated by function with 5 to 10 clinical specialties; size ranges from 200 to 800 beds; often referred to as a provincial hospital. Alternative term: General hospital-Regional hospital-Provincial hospital (or equivalent administrative area such as county)
Tertiary-level hospital: highly specialized staff and technical equipment— for example, cardiology, intensive care unit, and specialized imaging units; clinical services highly differentiated by function; could have teaching activities; size ranges from 300 to 1,500 beds. Alternative term: General hospital -National hospital -Central hospital -Academic or teaching or university hospital
Source: Definitions from Mulligan and others 2003, 59.
